Have you ever wondered what estrogen does and how it affects bone health?
We tend to think of estrogen as the female hormone, which it is, but men also have and need a certain amount of estrogen just as women need a certain amount of testosterone. In women estrogen has an important role in all things related to reproduction. Estrogen is involved in the initial sexual development of girls at puberty, and then throughout a woman’s life estrogen regulates the female menstrual cycle, supports growing babies during pregnancy along with progesterone, and affects female mood and serotonin levels. Estrogen also affects urinary health, the heart, blood vessels, skin, hair, pelvic muscles, and lipid, also known as fat metabolism. Estrogen also has an important impact on protecting bones for both women and men.
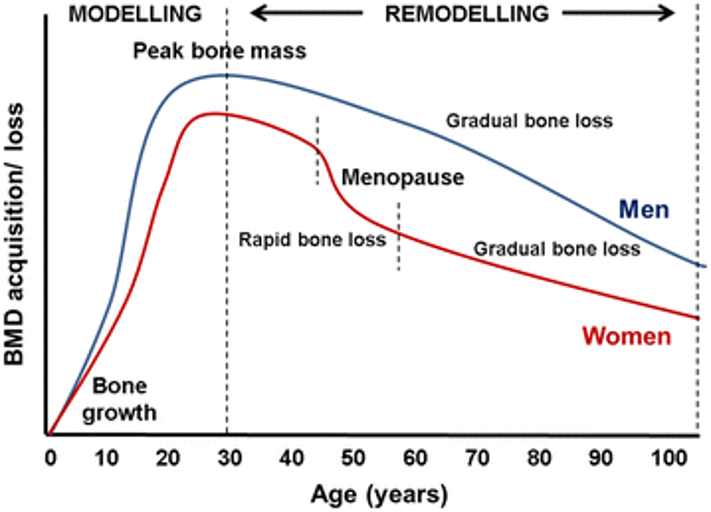
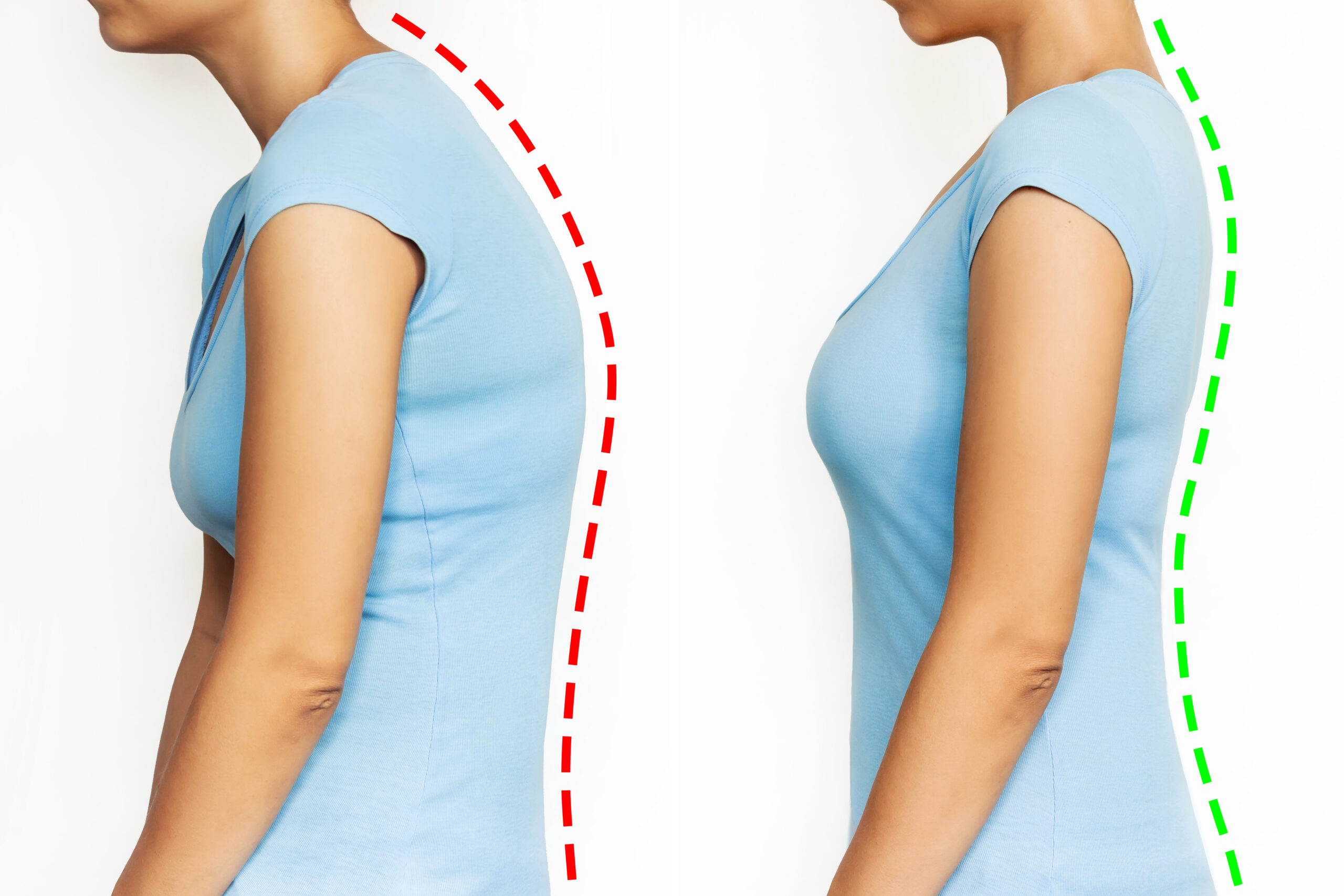
It is also likely that you have heard that when a woman enters menopause that she has a large drop off in estrogen that causes her to lose a lot of bone in a hurry.
Why this is a problem? Afterall menopause is a natural part of life, right?
When a person has low levels of estrogen, problems can arise.
- Hot flashes
- Night sweats
- Breast tenderness
- Vaginal dryness
- Mood swings and irritability
- Painful sexual intercourse
- Decreased libido
- Irregular menstruation
- Depression and anxiety
- Fatigue
- caused by disrupted sleep
- Brain fog
- Headaches
- Thinning hair
- Digestive issues
- Constipation
- Gas and bloating
- Slower digestion
- Gut health issues
- Increased visceral fat or fat around the belly
- Rapid bone loss
Many of these symptoms are signs of menopause, but some are not things we may not necessarily associate with menopause like gut health.
How does estrogen affect our bones?
Estrogen has a moderating effect on our bones by keeping bone resorption, also known as bone breakdown in check. Basically, estrogen slows down how much bone our bodies break down.
Once a woman reaches menopause, and her ovaries stop producing estrogen there is a 2-4% drop in bone density per year for a period of approximately five to seven years. After menopause bone resorption, also known as bone breakdown, increases by about 90% from its premenopausal level and bone formation is reduced by about 45% from its premenopausal state.
Those are some serious repercussions for our bone health post menopause!
How can we increase estrogen naturally?
We can eat foods that have phytoestrogens in them that mimic estrogen. Our bodies recognize phytoestrogens as estrogen. Foods that have high levels of phytoestrogens include:
- Fruits such as berries, apples, pears, grapes, peaches, and plums
- Vegetables such as broccoli, Brussels sprouts, kale, and onions
- Grains such as wheat, oats,and barley
- Nuts and seeds including peanuts, almonds, sesame seeds, and sunflower seeds
There is also a special class of phytoestrogens called isoflavones. The best source of isoflavones is soy. This includes miso, soybeans, and tofu. Other good sources of isoflavones include red clover, chickpeas, peanuts, green tea, split peas, lima beans, fava beans, lentils and flaxseeds.

Another natural way to boost estrogen is to get enough of the vitamins and minerals that help estrogen levels. The vitamins that are helpful for improving estrogen levels are vitamin D, vitamin B, and vitamin E. Boron is a trace mineral that helps our bodies absorb estrogen.
What about hormone therapy for estrogen?
Hormone replacement therapy may not be appropriate for everyone, and it is important to talk to your doctor about whether you are a good candidate for hormone replacement therapy. If you have had cancer, heart or liver disease, high blood pressure, or a history of blood clots, hormone therapy is not a good option for you.
For many women- not all women- ultra low dose hormone replacement therapy is a good option. A scientific study titled “Effects of ultra-low dose hormone therapy on biochemical bone turnover markers in postmenopausal women: A randomized, placebo-controlled, double-blind trial” published in 2022, found that women receiving E2 Estradiol, in the amount of .5 mg daily given orally developed a protective effect on their bones and bone resorption was slowed.
Healthy postmenopausal women who had a uterus between the ages of 45 and 60 were recruited for the study. The exclusion criteria for the study included women who had undergone a surgical menopause, had previously taken oral hormone therapy, had cervical or breast cancer, type two diabetes, high blood pressure, heavy smokers, took blood thinners, thyroid medication, glucocorticoid steroids, immunosuppressive drugs, and bisphosphonates within the past twelve months.
It is worth pointing out that ultra-low dose hormone therapy may still be appropriate for some people who are in the exclusion category for this study. When studies are performed it is important to try and keep the variables as small as possible to determine the accuracy of the results of a particular study. In this case all the different health care scenarios are variables. It may still be appropriate to do ultra-low dose hormone therapy with some of these health situations. Cancer and high blood pressure are reasons to not do hormone replacement therapy.
The study was conducted over a 24-week period. It was set up with 59 people receiving ultra-low dose hormone replacement therapy and 60 women in the placebo group. The study was double-blind meaning the participants and the researchers were unaware of who received actual hormones and who did not.
Women who received E2 in the amount of .5 mg daily had a significant reduction of their P1NP marker from the baseline that was taken while those women in the placebo group did not see a significant change in their P1NP marker.
The P1NP marker is one measure of new bone formation.
Here is a quote from the study conclusion, “Our results suggest benefits in the prevention of osteoporosis in young postmenopausal women with ultra-LD HT. (low dose hormone therapy) For women with less severe symptoms, ultra- LD HT may be sufficient to control symptoms.”
It is exciting that researchers see the potential for ultra-low dose hormone replacement therapy to be all that is needed to treat bone loss for many women.
When talking about hormone replacement therapy, the Women’s Health Initiative from 2004 also needs to be addressed. For many people the results from this initiative left created concern that hormone replacement therapy was not a good option and could potentially lead to heart health complications. It is important to recognize that there was a limit in the scope of this initiative and that further study has been done since the initiative. Women who have had cancer, have high blood pressure, type two diabetes, or another heart related complication are not considered candidates for hormone replacement therapy. The other thing to recognize is that what is being recommended is also different from what was being looked at. Hormone replacement therapy in the general sense is different in its dosing from ULTRA LOW DOSE hormone replacement therapy. So, the dose given is different and the people who are candidates are considered more carefully.
Estrogen is an important topic when looking at bone health and how to improve it. If you consider doing hormone replacement therapy look into ultra-low dose hormone replacement therapy and make sure that the doctor you work with has a firm understanding of the difference of approaches.
If you would like to learn more about this topic check out The Bone Builder System’s YouTube video, “The Impact of Estrogen and HRT on Bone Health Explained”
References:
https://pubmed.ncbi.nlm.nih.gov/8852944
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8836058/.
https://my.clevelandclinic.org/health/diseases/22363-high-estrogen
https://academic.oup.com/jcem/article/99/4/31A/2537122
https://www.urmc.rochester.edu/encyclopedia/content.aspx
https://zoe.com/learn/low-estrogen-in-women
https://www.health.harvard.edu/newsletter_article/isoflavone-content-of-selected-foods
https://www.uclahealth.org/news/article/3-ways-increase-estrogen-naturally
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9500172